History of This Rare Disease
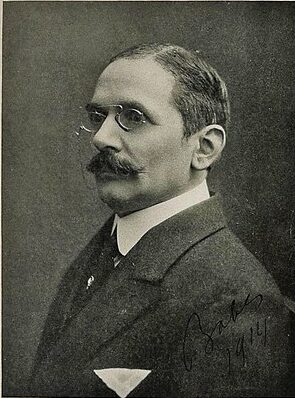
The parasite Babesia was named after Romanian scientist Victor Babes, who was the first to discover babesiosis pathogens in the red blood cells of cattle in the year 1888. Later in 1892, he observed similar organisms in sheep blood [3]. Babes was a prominent physician and one of the first few bacteriologists in the world. He is also considered one of the founders of modern microbiology and the second radiologist in the world (after Louis Pasteur) to introduce rabies vaccines into Romania.
In 1893, Smith and Kilborne in the United States also identified similar organisms in cattle blood that were later called Babesia bigemina and found to cause cattle fever. Over time, more than 100 babesia species have been identified in animals [4].
The first case of human babesiosis was identified in 1957 in a farmer in Croatia (at the time, a part of Yugoslavia). The farmer presented with fever, anemia, and hemoglobinuria. At the time, the causative agent was unknown but was later found to be B.divergens [4].
Since then, several other species of babesia causing infections in humans have been identified. Of these, B. microti, B. duncani, and B. venatorum are the parasites responsible for the majority of cases in humans [5].
B. microti was first identified in an immunocompromised person in the US in 1969 [5]. B. duncani was also identified in the United States in 1991 [6]. In 2003, B. venatorum was identified in Italy [2,4].
Together, these four babesia species are confirmed to be zoonotic pathogens [2].